More than 400,000 Kiwis live with eczema, an incurable skin condition that can cause itchiness, discomfort and pain.
One sufferer says sometimes the itchiness is “unbearable” and has caused him to miss work or have to go to the emergency department for infections – but that’s not even the worst part.
Tauranga eczema sufferer Luke Tucker has tried “hundreds” of treatments to ease the itching caused by his “full-body” skin condition.
The 21-year-old has used steroid creams but when he went “cold turkey” on a doctor’s advice, the withdrawal symptoms were “far worse” than having eczema.
His skin became “cracked”, dry, and infected, he says.
“It was the worst flare-up I’ve ever had. That was when I got all my infections across my body.”
Luke has since found an oral medication - Methotrexate - has been the most effective.
“It kind of suppresses my immune system so my eczema doesn’t come up as much.”
 Tauranga eczema sufferer Luke Tucker. Photo: NZME.
Tauranga eczema sufferer Luke Tucker. Photo: NZME.
Eczema is the most common chronic inflammatory skin disease. About 212,000 adults and 193,000 children live with the non-contagious condition in New Zealand.
Symptoms of eczema include itchiness, discomfort, loss of sleep and raw, sensitive skin causing pain.
There is no cure for eczema. Over-the-counter and prescription treatments are available to help manage symptoms, but results vary from person to person and can depend on severity.
Luke is sharing his story as a survey, commissioned by the Eczema Association of New Zealand and pharmaceutical company AbbVie, found 75 per cent of sufferers says available treatments were ineffective at bringing an eczema “flare-up” under control.
The report says eczema was the result of an overactive immune system. While the main cause of eczema is unknown it was thought to be influenced by the combination of genes and environmental triggers, such as stress, some foods and alcohol, as well as irritants such as weather and allergens.
‘Sometimes I can’t go to work’
Luke tells the Bay of Plenty Times he was diagnosed as a child, experiencing itchiness behind his elbows and knees.
As he got older, his eczema got worse, becoming “a full-body thing”.
“I’m always itching.”
Luke had flare-ups three or four times per year when he would get “quite a lot of scabs and open wounds”.
“Sometimes I can’t go to work or I don’t want to go outside.”
Luke - who works for his parents’ business as a cook - estimated he missed about two weeks of work each year due to flare-ups.
As a student, he had missed school sometimes because his eczema was “unbearable”.
‘I couldn’t even walk’
Luke was hospitalised for his eczema earlier this year when he woke up and “my whole calf was purple” due to an infection.
“I couldn’t even walk on it.”
His doctor prescribed him some “pretty hardcore” antibiotics and he was “stuck in bed for a week”.
But the infection got worse and spread to his thigh.
He went to the Tauranga Hospital emergency department, where he was prescribed stronger antibiotics.
Luke says doctors told him the infection probably came from his eczema due to having open wounds on his leg.
“That’s the worst infection I’ve ever had.”
 Luke Tucker's leg when he had an infection caused by eczema. Photo: NZME.
Luke Tucker's leg when he had an infection caused by eczema. Photo: NZME.
Luke says, in his view, the worst problem relating to eczema was the wait times to see a dermatologist.
He was told the wait time for an appointment publicly was nine months. Privately was six months.
Luke says he paid to see a private dermatologist, with a 10-minute appointment costing between $400 and $500.
He says steroid creams had been the most effective treatment until the dermatologist prescribed him a “steroid immuno-suppressant” - Methotrexate - three months ago.
Luke says it was meant to take six to 12 months to be fully effective but he was already noticing a difference.
His eczema was “much easier” to manage now and he did not have to use his steroid creams as much.
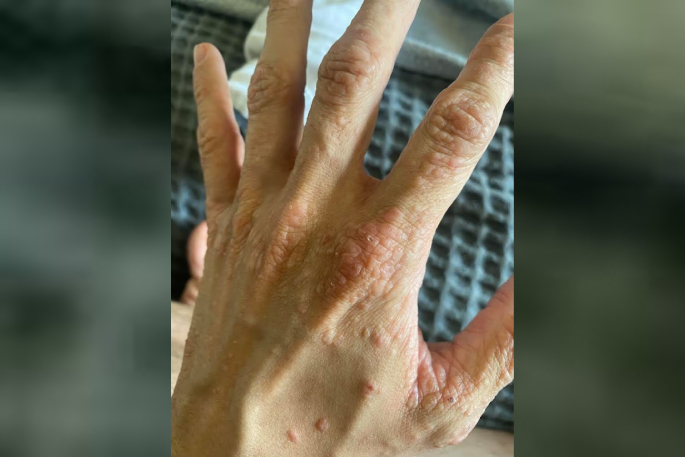 Tauranga man Luke Tucker says his eczema got worse as he got older. Photo: NZME.
Tauranga man Luke Tucker says his eczema got worse as he got older. Photo: NZME.
Luke says the downside of steroid creams was the withdrawals if he stopped using them.
As a teenager, he saw a dermatologist who advised him to stop using steroid creams and prescribed him “more natural” alternatives.
Luke says he went “cold turkey” and had infections all over his body.
He tried antibiotics but only steroid cream worked.
Luke says he had tried “hundreds” of natural treatments but none of them had helped, especially during a flare-up.
Pain and ‘sleepless nights’
A joint press release from the Eczema Association of New Zealand and AbbVie says 51 per cent of adults surveyed reported the condition had a moderate to significant negative impact on their daily lives.
It also found 97 per cent of Kiwi adults with eczema says it negatively impacted their mental health, including low self-esteem, stress, depression and anxiety.
The association hoped the report would prompt more understanding and compassion for eczema patients.
Eczema Association of New Zealand spokeswoman Vanessa Jenkins says eczema was often described as a “hidden disease”.
“But it has a very real physical, emotional, economic, and social toll on patients and their families.
“It’s a life characterised by pain, sleepless nights, personal and social anxiety, a deep sense of helplessness and loss of confidence from never being on top of the condition.”
Country head of AbbVie New Zealand Bronwen Marshall says it estimated the productivity loss from workplace absences due to eczema was up to $299 million each year.
She says people faced challenges in accessing care and treatment. Waiting lists for public dermatology services were long and cost could be a barrier for some accessing private services.
Dermatologists ‘a very small and specialised medical workforce’
Health New Zealand director of programmes delivery unit for hospital and specialist services Duncan Bliss says, like many specialty services across the health system, dermatology was experiencing staffing challenges throughout the country.
Bliss says dermatologists were “a very small and specialised medical workforce” and accounted for about 30 people nationally (about 22 fulltime equivalent staff) in the public health system.
Health New Zealand was taking steps to support the growth and retention of its medical workforce, including senior medical officers of which dermatologists were included, he says.
Bliss says dermatology services were generally made up of multi-disciplinary teams, including consultants, registrars, nurse specialists, and dermatology nurses.
Patients were seen by doctors and nurses throughout their care including, primary care, hospital-based community teams and hospital services.
“As always, patients are prioritised based on clinical need, with those needing urgent care seen first, followed by semi-urgent and routine referrals.
“Further work is under way to develop training opportunities for clinicians and to introduce systems or technologies which increase the speed and capacity of the service.”



0 comments
Leave a Comment
You must be logged in to make a comment.