Grieving families, overworked ambulance staff, and rising complaints. Did the recent funding boost for a critical emergency service go far enough? Tara Shaskey talks to families who say more needs to be done to improve our ambulance services.
An email containing an apology from an ambulance call handler following the death of Leanna Petherick’s teenage daughter sits in her inbox.
It is coming up five months since it arrived but she cannot bring herself to open it.
“I left it. I haven’t been able to read it. I don’t want to know. I’m going to get a friend to do it but I’m just not ready,” Petherick says, her voice breaking with emotion.
It has been four years since 17-year-old Tayla Brown died at their Tauranga home on July 23, 2020, following an asthma attack.
It had taken two desperate calls to emergency services and a 28-minute wait before paramedics arrived and, by then, it was too late.
A recent report by the Health and Disability Commissioner (HDC) found the ambulance was not sent as urgently as it should have been.
Petherick’s loss has devastated her beyond measure, but she says the emergency services call handler, breached by the health watchdog, “is only human” and “made a mistake”.
The grieving mother instead believes there is a systemic problem at play and that responsibility lies at the feet of the services’ top brass and those who fund them.
Tayla’s death is one of several highlighted through HDC and coronial investigations into potential failures by Hato Hone St John and Wellington Free Ambulance in recent years.
The most recent report was in October when the HDC released findings into a man who died as his wife drove him to the hospital in 2020.
He was suffering “classic heart attack symptoms” but St John still had not dispatched an ambulance almost an hour after the first 111 call was made.
Complaints rise but so do calls to 111
According to HDC figures, the health watchdog received 166 complaints involving Hato Hone St John from July 1, 2019, to June 30, 2024.
For that same period, St John received 3.1 million calls and responded to 2.1 million. While the number of annual complaints about the service fluctuated over that time, they almost doubled from 26 in 2019/20 to 49 in 2023/24.
Typically, they made up only around 1% of annual complaints to HDC, whose complaints process now has greater public awareness than in previous years.
A delay in treatment was the primary issue for 38 of the 166 complaints received.
During the same period, HDC closed 126 complaints and referred them back to St John to engage with the complainant or found that the care was appropriate. However, 11 complaints were formally investigated, three of which involved delays in service provision.
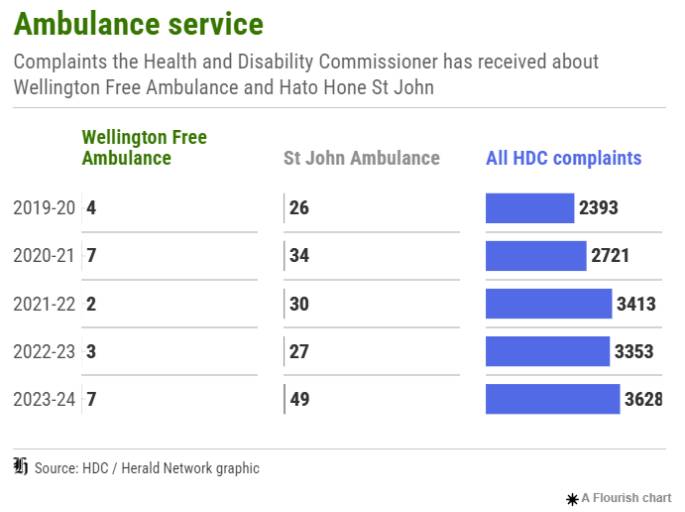
Overall, four investigations resulted in St John being found in breach of the Code of Health and Disability Services Consumers’ Rights. Two of those complaints involved the death of a person. One - the man who died on the way to the hospital - resulted in St John being breached for failing to meet expected wait times.
Five complaints led to breach findings against individual St John staff, including five paramedics and one non-clinical administrator.
There are currently 51 open complaints involving St John, including one formal investigation. Of those, a delay in treatment is the primary issue in 16 of them.
For that same five-year period, HDC received 23 complaints involving Wellington Free Ambulance, which provides free ambulance and healthcare services for the Greater Wellington and Wairarapa region.
Nine of the complaints remain open, including one that is under investigation. HDC closed three investigations into care provided by the service during that period, with two involving the death of a person, one of which resulted in a breach of the code.
‘I gave birth to her and I lost her’
In Tayla’s case, the call handler failed to understand, and clarify, the degree of difficulty she was having breathing. The call handler then incorrectly coded the priority of the ambulance as Orange1, when it should have been Red1.
The allocation of Orange1 allowed for the immediate dispatch of an ambulance but a dispatcher then failed to send a nearby, available ambulance to her home. The ambulance was instead sent on a break.
While the May HDC findings made an adverse comment about the actions of the dispatcher, who was employed by St John, the call handler, who worked for Wellington Free Ambulance as the organisations share call centres, was found to have breached the code. Neither of them remain in their roles.
 Tayla with her mother, Leanna Petherick, and sister, Tuesday. Photo supplied.
Tayla with her mother, Leanna Petherick, and sister, Tuesday. Photo supplied.
The HDC also made an adverse comment about St John’s staffing levels, after the dispatcher revealed his area was often understaffed and no one was available that night who he could escalate the decision to.
While inadequate staffing levels at St John, personnel burnout, and funding shortfalls have long been in the spotlight, recent headlines around strike action and continued pleas for better pay and more Government funding have underscored the concern.
In October, the Government committed to giving St John a $21 million boost, increasing the overall funding to almost $357 million, or about 86% of costs, met through Te Whatu Ora - Health New Zealand and ACC. But the contribution will go towards inflationary pressures - and a gap will remain.
It is a gap that has seen renewed union calls for the Government to fund 100% of the service, with concerns that without it, it will continue to be under-resourced and delays and risks to patient outcomes, including more deaths, will persist.
However, the Government has seemingly dismissed the idea of funding the critical service outright.
The funding shortfall continues to be made up through donations, fundraising and a part charge of $98 for patients transported by ambulance.
For Petherick, who recently flew to New York with her younger daughter to mark what would have been Tayla’s 21st birthday, she acknowledges the services have made changes, including around training, in response to the death of her daughter.
But that night continues to haunt her and she has lost faith in the critical healthcare service.
She says ensuring accountability and further improvements in the system is essential in honouring Tayla’s memory and preventing further loss.
“I could have been at the hospital in five minutes and she could have had a better chance. So how does that make a parent feel? I wish I had done things differently.
“She was left alone with her mum trying to give her CPR and compressions not knowing what she was doing to keep her alive.
“I gave birth to her and I lost her.”
‘Joyful and always laughing’
Petherick’s pain and frustration are all too familiar to Eli Tapuvae.
His mother Sharon Solofua Tapuvae, 54, died of an acute heart condition at her Auckland home on July 29, 2021.
After Sharon collapsed, her husband phoned for an ambulance five times only to be told none was available.
Then Eli called, just over an hour after his father made the first call, to say his mother was not breathing.
 Sharon Solofua Tapuvae, 54, died at her Auckland home in 2021. Photo supplied.
Sharon Solofua Tapuvae, 54, died at her Auckland home in 2021. Photo supplied.
Her husband started CPR and an ambulance was dispatched. About 15 minutes later, she had no pulse and had gone cold.
Ambulance personnel arrived and continued resuscitation but she could not be revived.
A coroner said in findings released in late 2023 that it was impossible to conclude whether Sharon would have survived had an ambulance been dispatched more quickly but she was “very concerned” at the lack of ambulance availability.
She said the death highlighted the serious and distressing impacts that could occur when there were insufficient ambulance resources in communities, and recommended St John lobby the Government for more funding.
The coroner also recommended the service consider whether changes were needed to improve communication with callers who may not speak English as their first language, with the findings noting Sharon’s husband may have had difficulty understanding some of the questions asked when he phoned 111.
In another case, Rangiora woman Margaret Wells died after a 70-minute wait for an ambulance after her double amputee husband, Alfred, called for help.
A coroner released findings into the 2020 death in April 2024, describing the circumstances as “deeply troubling” and saying that despite Alfred calling St John concerning a life-threatening medical emergency, it took more than an hour for paramedics to arrive “due to scarce ambulance resources and competing demands”.
 Margaret Wells, pictured with her husband Alfred, died after waiting 70 minutes for an ambulance. Photo supplied.
Margaret Wells, pictured with her husband Alfred, died after waiting 70 minutes for an ambulance. Photo supplied.
As Eli continues to mourn his mother, even seeing an ambulance on the street upsets him.
It takes him back to losing his mother, who he describes as God-fearing, joyful and always laughing.
“I don’t think I’ll ever get over the loss of my mum, but I get stronger every day, I guess.”
Eli never lodged a complaint with HDC, though he did seriously consider it.
“At the end of the day, I felt like it wouldn’t have much of an impact. And it won’t bring my mum back.”
However, he hopes to see continued improvements within the service, particularly around better response times, so no other families experience the tragedy he has.
“More ambulances should be available … it’s a necessary service for a country like ours. We’re not living in the bush.”
Ambulance fleet and workforce grows
Associate Health Minister Casey Costello noted the coroner’s recommendation around funding and pointed out there had been “a very large increase” since Sharon’s death, as well as an improvement in response times.
“In the last three years, the emergency ambulance providers, Hato Hone St John and Wellington Free Ambulance, have received an extra $261 million in funding.
“The joint contract that Health NZ and ACC have with those two services currently provides nearly $405 million a year in total, with Hato Hone St John to receive around $357 million this year.”
Costello was aware of union calls for 100% funding, but said that would ”significantly alter the relationship with the organisations”.
“Both providers augment their revenue with donations, fundraising, and sponsorship and are known and trusted organisations in the community.”
 Associate Health Minister Casey Costello says there has been an improvement in ambulance response times. Photo / Mark Mitchell.
Associate Health Minister Casey Costello says there has been an improvement in ambulance response times. Photo / Mark Mitchell.
Wellington Free Ambulance chief executive Dave Robinson said the charity had to raise more than $8m a year to bridge the funding gap and keep services free.
The organisation’s staff took on a huge responsibility in their roles and always worked hard to do their best for the community.
But the reality, he said, was that it was increasingly challenging to balance the needs of the community, the people, and the service with current resourcing levels.
“Wellington Free Ambulance welcomes the opportunity to discuss long-term sustainable funding with Government.”
Jon Moores, Hato Hone St John head of clinical governance, said he was grateful for the increased funding contribution and the relief it would bring to inflationary pressure. But there was still a gap.
Moores said St John was “continuing to work” with the Government to address the difference between what it costs to run the ambulance service and the funding it receives to ensure that is covered in the next contract, which begins in 2026.
However, he echoed Costello, saying that despite the increasing demand on the health system, those with life-threatening emergencies were getting faster response times from St John than in the past three years.
In 2022, the average response time for that level of emergency was 16.19 minutes while it currently sits at 13.40 minutes.
Moores said the ambulance fleet had also grown, as had the workforce.
“We currently have more than 1800 frontline ambulance personnel in place. This is 100 more frontline personnel than the same time last year, and 270 more than two years ago.”
Any delays in the service’s response times resulting in patient harm were “incredibly upsetting”, he said.
“But we also recognise that increasing demand on the wider health system can impact the availability of ambulances, contributing to delays and we sincerely apologise for that.”
First Union national ambulance co-ordinator Faye McCann said that despite the noted improvements, the service was still “inadequately staffed”.
She still hears of ambulance officers having delayed breaks, not finishing on time and facing burnout.
“They are receiving constant text messages on their days off offering them shifts to come back in to work and cover; this is evidence of an inadequately staffed ambulance service.
“There are limited options available to patients in a life-threatening emergency and this is why it is so vital to have a well-funded and a well-run ambulance service - patients do not have any other choice.”
In September, First Union launched a petition to call for 100% government funding of ambulance services.
McCann said it did not make sense to have the service one step removed from the rest of the country’s critical healthcare services.
“It is important for the Government to step up and fully fund the ambulance service so we don’t keep hearing of delays and issues resulting in deaths. New Zealanders need a fully funded ambulance service. Such a crucial service should not be operated as a charity.”




1 comment
More funding
Posted on 10-01-2025 09:48 | By rogue
Let's not forget also that when you call for an ambulance to a heart attack you have a fire truck turn up as well.
Perhaps it's time to merge the fire service with ambulance like they do in most countries around the world.
Save money on ambulance and fire stations with cohabitation, less money on separate uniforms, less managers, less support staff.
Less money on fluff to spend on patients ... oh and probably more front line staff to keep up with aging population and immigration.
Leave a Comment
You must be logged in to make a comment.